Osteoporosis happens when resorption of bone minerals to the bloodstream occurs at a rate that exceeds bone formation - deposition of minerals in the bone. Bone remodeling happens continuously and in a healthy young adult the rates of deposition and resorption is about the same.
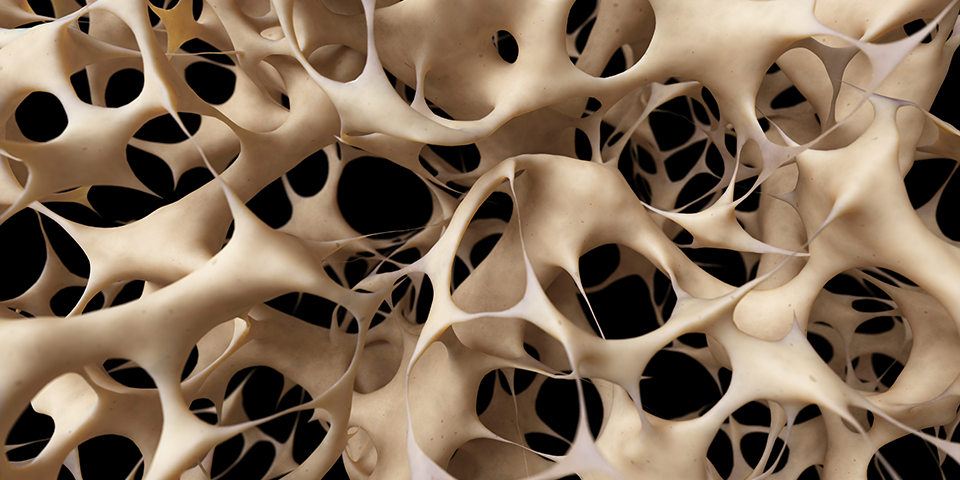
There are three types of bone cells: osteoclasts, osteoblasts, and osteocytes. Osteoclast cells resorb bone, and osteoblast cells form new bone. An imbalance in bone resorption as compared to bone formation can lead to osteoporosis. The problems are more serious usually in cancellous bones because the rate of bone formation is lower, especially among those suffering from osteoporosis.
 Usually between the ages of 40 and 50, both sexes experience some cortical bone loss as the rate of resorption exceeds the rate of bone formation. For women, this process often becomes more severe around menopause. After menopause remodeling activity in bones increases and a greater proportion of bone is remodeled on its endosteal (inner) surface.
Usually between the ages of 40 and 50, both sexes experience some cortical bone loss as the rate of resorption exceeds the rate of bone formation. For women, this process often becomes more severe around menopause. After menopause remodeling activity in bones increases and a greater proportion of bone is remodeled on its endosteal (inner) surface.
The measure of osteoporosis also depends on peak adult bone mass that is usually reached around age 30 - possibly earlier for trabecular bone. Trabecular bone is the spongy bone tissue found at the end of vertebrae and long bones, while cortical bone is the outer shell and middle of long bones. If peak bone mass is low, i.e., one does not develop a strong skeleton during youth, then bones may become fragile more quickly with the onset of osteoporosis.
The role of menopause in osteoporosis is tied to the decrease of estrogen levels, which results in an an increase of bone resorption and a decrease of new bone formation. The parathyroid gland can also contribute to bone loss if excessive parathyroid hormone is released. A lack of dietary calcium and vitamin D can impair calcium metabolism and further aggravate the body’s ability to form strong new bones. Smoking and excessive alcohol consumption have been identified as contributing risk factors for osteoporosis. Use of prescription steroid medications also can cause osteoporosis.
Interestingly, bones that bear weight - such as spinal bones and legs - are more apt to get osteoporosis than the skull, which bears little weight and functions largely to protect the brain. Some scientists think that if they can understand at a micro level the differences between these types of bone - that this understanding will lead to treatment or prevention of osteoporosis.\
A study by the Max Delbrück Center for Molecular Medicine (MDC) Berlin-Buch, Germany suggests that there is a genetic link to the pathogenesis of osteoporosis. The researchers found that two types of a gene switch determined the balance between bone formation and bone resorption. A short isoform and long isoform of the gene switch are suggested to play a major role in this process. The long isoform is thought to suppress osteoclasts from resorbing bone, while the short isoform promotes bone resorption.
When osteoporosis occurs, the bone can weaken due to the loss of density to a point in which they can no longer support normal activity. In such cases, bone fractures can occur from minor incidents including light falls. The strength of the bone though is not just a matter of density but also the quality or structure of the bone.
Sometimes the term secondary osteoporosis is used to refer to refer to osteoporosis that can be traced (or at least strongly suspected) to another cause such as medicine use (e.g. steroids).
Several years ago scientists discovered that serotonin produced in the digestive system influenced bone strength and that more serotonin resulted in weaker bones. Mice bred to not produce this serotonin had extra strong bones. This led to interest in developing methods to approach bone strength through this serotonin pathway, although so far this route has not produced any treatments.
Growing up healthy establishes good bone quality that will help prevent the slip into osteoporosis in the elderly years. Good nutrition and exercise can help kids build bone density. Public health officials often express concerns about children getting insufficient exercise and about the disappearance of physical education classes in schools. Maximum bone density is achieved in the mid to late 20s.
When pregnant, women often lose bone density. The calcium demands of the growing fetus are given priority. The effect on the mother's skeleton continues through breastfeeding and this is a time of accelerate bone turnover. After the child is weaned the bones return to normal, until the next pregnancy. It is impossible to notice changes in the skeletal system in both pregnancy and menopause and not think about the effect of hormones.
Comorbidity sounds scary but it is just a word that means you have two diseases at the same time. Diabetes is often co-morbid with osteoporosis. The federal government says that women with lupus are significantly more likely to get osteoporosis.
It’s not clear why this is. The medications used to treat lupus promote bone loss, so that is part of it. And the pain and discomfort of lupus make women more likely to be sedentary. Women make up most lupus patients as they make up most osteoporosis patients. We have not been able to find any scientific studies that suggest a plausible connection between the pathogeneses of the two diseases.
Spanish: Patogénesis de la Osteoporosis

