Osteoporosis can be caused by the use of synthetic corticosteroids. Corticosteroid-based medications are used to treat wide variety of diseases including skin conditions, asthma, brain tumors, and adrenal insufficiency. Inflammatory diseases produce elevated levels of cytokines in the bloodstream, and that condition is also associated with increased risk of osteoporosis. So some cases of steroid-induced osteoporosis may be partly due to osteoporosis caused by the underlying condition that the steroid medicines are given to treat.
Glucocorticoids naturally produced in the body can also contribute to osteoporosis, and it is excess glucocorticoids developed during Cushing’s disease that make that disease cause bone loss.
Bone demineralization happens within a few months of when a patient starts taking the steroid.
Steroid-induced osteoporosis is often debilitating. It is characterized by excruciatingly painful bone fractures. The risk for osteoporosis goes up with increased dosage of steroids. Fracture risk declines after the person stops taking the steroids.
This is the most common form of secondary osteoporosis and among people under age 40, it is the most common form. Medical literature sometimes refers to this condition as Glucocorticoid-induced osteoporosis (GIOP).
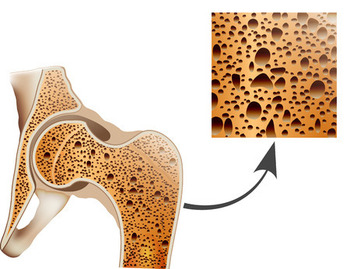
Like other forms of osteoporosis, this type is a "silent disease" until a bone break occurs. The signs that might suggest steroid-induced osteoporosis are: Inhibition of calcium absorption in the digestive system, reduction of urine calcium, inhibition of osteoblast function and enhancement of bone resorption
Bone density lab testing procedures are the same as in the case of age-related osteoporosis. However, scientists have found a weaker correlation between bone density and fracture risk in steroid-induced osteoporosis than in the more common age-related type.
Doctors who suspect steroid-induced osteoporosis in women typically inquire about the menstrual cycle. An absence of menstruation is an even stronger indication of the disease than estrogen deficiency. Male patients should have their testosterone levels checked. Calcium levels in the urine are checked for hypercalciuria (too much calcium), which may be a result of bone resorption. To see if hypercalciuria is related to the bone destruction the doctor checks urine N-telopeptide (NTx) levels.
PTH and 25-hydroxyvitamin D levels are checked in the patients with very low bone density or bone fractures and in patients with high steroid dosage intake.
X-rays of the spine are used to diagnose steroid-induced osteoporosis in patients put on long-term corticosteroid treatment because their spinal bone fractures may not be detectable by other means.
Side effects of synthetic corticosteroids depend on the patient’s underlying condition, medical history, age, sex, metabolic rate and variety of other factors. It is practically impossible to predict how long a patient will be taking corticosteroid-based medications before he or she develops steroid-induced osteoporosis.
Monitoring of the patient’s body conditions is important. Experienced doctors decide which diagnostic procedures are appropriate for each patient, and how often medical testing should be done. In may happen that the doctor decides that the patient should decrease the intake of medications, or even stop the treatment and seek other alternatives not involving corticosteroids.
The American College of Rheumatology recommends patients on these drugs take calcium and Vitamin D supplements. Patients at moderate-to-high fracture risk should also take a bisphosphonate medicine as a preventative.
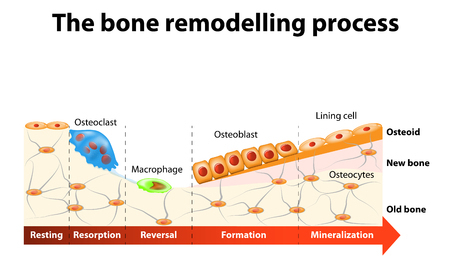 Steroid-induced osteoporosis is approached differently from other forms of osteoporosis. For example, anti-resorptive therapy, which is effective in treatment of postmenopausal osteoporosis, does not always produce the desired bone density increase in patients with steroid-induced osteoporosis.
Steroid-induced osteoporosis is approached differently from other forms of osteoporosis. For example, anti-resorptive therapy, which is effective in treatment of postmenopausal osteoporosis, does not always produce the desired bone density increase in patients with steroid-induced osteoporosis.
Treatment of steroid-induced osteoporosis begins with the patient taking calcium supplements of 1 to 1.5 gm/day. For patients with hypercalciuria, doctors often prescribe low-dose thiazide diuretics to promote calcium intake by reducing hypercalciuria.
The American College of Rheumatology recommends treatment with bisphosphonates.
People used to worry about heartburn medicines. An investigation into the effects of proton-pump inhibitors used for control of acid-reflux disease (bad heartburn) found no statistically significant increase in osteoporosis risk.
The anticoagulant medicine heparin has many medical uses and if used for long periods of time, it can increase the risk of osteoporosis.
Spanish language page - Osteoporosis Inducida por Esteroides
Scientific abstract: Glucocorticoid-induced osteoporosis: an update on current pharmacotherapy and future directions.