In the elderly years, people often experience weight and muscle loss, declining endurance, diminishing balance, waning mobility, and an overall decreased levels of activity. A combination of these symptoms marks Frailty Syndrome.
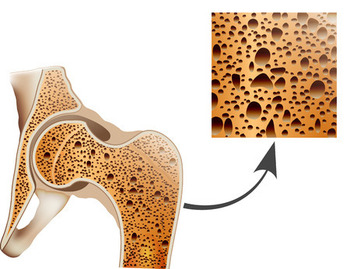
Frailty syndrome is also called musculoskeletal frailty although frailty affects both the musculoskeletal and nonmusculoskeletal systems in the body. The word sarcopenia refers to age-related muscle loss. It is the muscle analog of osteopenia, which is thinning of the bone. The focus of frailty syndrome for doctors is often sarcopenia.
The hallmarks of this syndrome include the deterioration of physiological systems that - when occurring simultaneously - increase vulnerability to abrupt negative changes in health status following mild physical or emotional trauma. Now considered a clinical syndrome that can be diagnosed through lab tests and a doctor's office visit, frailty syndrome is increasingly being recognized by doctors and other caregivers.
People with frailty syndrome have an increased risk of cognitive impairment, and those with mild cognitive impairment or dementia are more likely to develop frailty syndrome. Some scales employed to diagnose frailty include cognitive status.
An early study in 2001 used this criteria: "Frailty was defined as a clinical syndrome in which three or more of the following criteria were present: unintentional weight loss (10 lbs in past year), self-reported exhaustion, weakness (grip strength), slow walking speed, and low physical activity."
How many people have frailty syndrome? It's hard to say. Different researchers have come up with different estimates. For people past age 65, the percentage is thought to be below 20 percent, but it could be as low as 5 percent. Among people in this age range with cancer, the prevalence is thought to exceed 40 percent.
Frailty syndrome leads to increased incidence of disease, illness, functional decline, and early death. People with the syndrome more often experience hip fractures, disability, and hospitalization than those without.
Frail people are at risk for falls, hospitalization, and physical disability. Complications associated with Frailty Syndrome include frequent falls due to poor balance and decreased muscle strength. Bone fractures are often the result. These injuries often take a long time to heal and rehabilitation is sometimes incomplete, leading to a cycle of frailty, permanent disability, and even mortality. Emotional or psychological stressors within the cycle of frailty can contribute to the decline of cognitive function as well as the onset of dementia. Insulin resistance often develops.
Frailty syndrome negatively affects quality of life. People with it are more likely to be depressed and have poorer perceptions of their own health than non-frail people.
Frailty is a true syndrome - a cluster of symptoms. It refers to diminishment in endurance, physical strength and activity, mental abilities, ability to maintain balance, and tendency of the person to take in adequate nutrition.
There is no widely used accepted diagnostic criteria for frailty. Some scientists have started using the "Fried frailty criteria" to establish whether a person has frailty syndrome. Factors considered include weight loss, handgrip strength, gait speed, level of physical activity, and tendency to exhaustion. So far this criteria has been used mostly by epidemiologists and not so much by doctors who treat patients.
Gait - or how fast a person walks - is a metric gerontologists look at in patient evaluation. Gait normally declines as a person gets older. If a person has dementia, it declines even more. People with dementia have lower blood flow in the brain. Brain injury - due to trauma or disease - is also associated with slower gait. Low cerebral vasoreactivity (i.e., changes in brain blood flow in response to changes in carbon dioxide in the air) is associated with slow gait speed and falls.
Also, slow gait speed is a sign of impairment in the ability to increase brain blood flow during cognitive tasks.
Sensory ataxia is a disorder where the balance function of the brain receives incorrect or incomplete information about location of the limbs. People with poor or disordered gaits have errant proprioception and trouble balancing. The Romberg test has been used for over a century to evaluate people (and has since been adopted to test drunk drivers). Nurses and therapists employ this test - which consists of asking the patient to stand unassisted with his or her eyes closed. Instability indicates neurological problems and suggest a propensity for falls.
Less acknowledged, but still considered by some, is pre-frailty syndrome. This is when the patient has some of the hallmarks of frailty syndrome. It does not have a firm definition, but clearly more people have per-frailty syndrome than frailty syndrome.
The prevalence of Frailty Syndrome is twice as high for women as for men. It becomes increasingly common in both sexes after the age of 65. The syndrome forms and progresses in a downward spiral during which the body’s ability to withstand and recover from illness or accidents dramatically declines. At the same time, due to aging, the body’s systems must spend increasing physiological reserves in order to function and recover from illness or accidents normally.
Often the frailty cycle begins with long-term poor nutrition. People don't get enough protein, carbohydrates, vitamins, and minerals. Poor nutrition leads to low energy levels and unintentional weight loss, along with deficiencies in the micronutrients necessary for combating illness. A lack of energy leads to decreasing activity and avoidance of exercise. Without consistent exercise muscle mass and strength deteriorate, along with cardiovascular functions. As a result, walking speed decreases, hand strength weakens, balance becomes compromised, and the ability to perform the everyday tasks of independent living fades.
These conditions encourage further reductions in activity level and consequently reduced energy expenditure. Appetite decreases even more and nutrition continues to be inadequate. As this downward spiral progresses the occurrence of a minor bacterial infection, emotional stress, or even changes in medication can lead to unpredictable complications. Like other geriatric syndromes, frailty produces physiological changes that result in the development of risk factors and more geriatric syndromes. The end of the spiral can be disability or even death.
You also sometimes hear of the "anorexia of aging" which is not the same as frailty syndrome although it has some similarities. Anorexia of aging involves the person eating substantially less and losing weight.
Frailty syndrome often looks like a vicious cycle. Once it gets going, the lowered capability of the person leads to less physical activity and further weakening. Then there can be a spiral of vertebral fracture, hip fracture, immobility, and loss of independence.
Risk factors for frailty syndrome are mostly the same as the factors for other conditions of the elderly. The biggest factor is advanced age.
The medical community has no consensus treatment regimen for frailty syndrome and doesn't even agree that it should be treated. Drugs under development include ones to stimulate hunger (so-called ghrelin agonists) and SARMs.
Preventative measures commonly recommended include: (a) maintaining adequate nutrition (especially Vitamin D and protein), (b) age-appropriate exercise, (c) administration of flu vaccines, and (d) monitoring daily living skill levels and equilibrium. Consistent structured exercise is the only method proven to slow the progression of the syndrome. Making the living space safer for frail people can reduce the risk of injury.
Here’s a new term to describe something bad: "osteosarcopenic obesity". It refers to a condition seen in old people who have (1) low bone density, (2) lost muscle mass, and (3) extra fat so they are classified as obese. This syndrome is more or less the co-existence of osteoporosis, sarcopenia, and obesity.
All three of these problems have been recognized for a long time. The underlying etiology of each may share factors and they make each other worse. It’s a case of negative synergy. According to some epidemiologists, the combination produces risk of “significantly worsened outcomes” than either one alone.
Fat infiltraton to intermuscular adipose tissue is one way gaining weight makes it difficult for older people to be mobile.
Spanish language version of this page.