Because neurons (nerve cells) in the central nervous system (the brain and spinal cord) do not repair or replace themselves after being injured, researchers are investigating whether transplanting cells into an injured area can restore function.
One of the many challenges for researchers is obtaining cells that will function as neurons in the brain or spinal cord. Because a person’s body doesn’t have spare neurons for transplantation, efforts are being made to find other cells that can be transformed into neurons. One potential source is “stem” cells from human embryos. Less than a week after conception cells in an embryo begin to “differentiate” – that is, they begin to form specific types of cells, such as bone cells, red blood cells, heart muscle cells, and so on. Stem cells are simply cells that can differentiate into other types of cells. Early in the life of an embryo stem cells have the potential to differentiate into the more than two hundred types of cells in a human body. There are other kinds of stem cells, including stem cells in adults, which can differentiate into a more limited number of types of cells.
Using embryonic stem cells for transplantation is controversial because it is necessary to first create human embryos to produce the stem cells and then kill the embryos in the process of “harvesting” the stem cells. Opponents of the process contend that it is unethical or immoral to create and then kill any form of human life for the purpose of harvesting stem cells. Proponents of stem cell transplantation either claim that embryos created in a laboratory have no value or significance apart from producing stem cells or that the end of helping injured or ill people justifies the means of creating and then killing human life.
Apart from the controversy about creating and killing human embryos, stem cell researchers are faced with another challenge which is partly practical and partly ethical. The body’s immune system recognizes what is part of the body and what is not. Every cell in the body has protein molecules on the surface of the cell wall that identify the cell as being part of the body (these are known as human leukocyte antigens (HLA)). These markers are recognized by the cells in our immune systems. If the immune system doesn’t detect the body’s specific markers, it will sound the alarm and go on the attack. This allows our immune system to recognize and fight invaders in the form of bacteria, viruses, and fungi, protecting us from diseases that would otherwise kill us.
However, this same ability of the immune system presents a serious problem when tissue from another person (or animal) is transplanted into the body. The immune system will ordinarily identify the transplant as foreign and begin to attack it. The attack is carried out by cells using chemical weapons that can kill other cells. This process is known as transplant rejection.
To prevent rejection two different strategies have been used. One is to find a transplant donor who has genetic markers (HLA) that are similar to those of the person receiving the transplant. The more similar the markers, the less likely it is that the immune system will reject the transplant. The other strategy is to administer drugs to transplant recipients that suppress the ability of the immune system to recognize and target transplants for destruction. While these drugs usually work, they have numerous side-effects and can make an individual more vulnerable to infections. Often times both strategies are used.
One potential solution to the problem of transplant rejection would be to create a transplant with markers identical to those of the person receiving the transplant. A person’s DNA contains the unique blueprint for that person’s body, including the details for the markers (HLA) that are recognized by the immune system. Some researchers are attempting to insert human DNA into cells that are then used to create human embryos. This process is known as cloning – that is, artificially producing another organism with DNA that is identical to the DNA of the “donor.” Cloning has been performed with some types of animals but not with a human being(1). If human cloning is eventually successful, the clone would have markers identical to those of the DNA donor. This would potentially allow transplants to be created with the DNA of the patient, which would be recognized by the immune system as belonging to the body. There would be no potential for transplant rejection and no need for drugs to suppress the immune system.
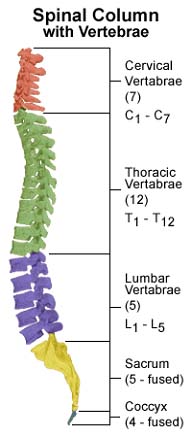
However, even if cloning is successful, researchers will still need to learn how to stimulate an embryonic stem cell to produce a neuron rather than a skin cell or some other type of cell. Transplanting undifferentiated stem cells runs the risk of creating a tumor, an event which has actually occurred when embryonic stem cells have been transplanted into mice. Furthermore, while finding a source of cells that can differentiate into neurons is one major challenge in developing a cure for spinal cord injuries, there are others (click on the “Treatments for the Future” link under the “Spinal Injury Treatment” tab.) Consequently, any effective treatment to repair spinal cord injuries using embryonic stem cells lies years, if not a decade or more, in the future.
Cloning is one example of genetic engineering, an activity in which people manipulate DNA to create organisms that wouldn’t otherwise exist in nature. While the first mammal (Dolly the sheep) was cloned in 1997, some clones have had health problems not characteristic of the species (including Dolly), are more prone to have offspring with birth defects, or have much shorter than normal life spans. The long term results of cloning are not known. As a result, ethical issues abound, and particularly when human cloning is the issue.
Given the difficulties, concerns, and controversy surrounding the proposed use of embryonic stem cells in transplantation, some researchers have investigated other types of cells. One promising source is olfactory cells, which are found in one of the nasal sinuses. These cells are already part of our nervous systems and function in our sense of smell. The olfactory cells include neurons, progenitor stem cells that can differentiate into neurons, and OEG cells (olfactory ensheathing glia cells; also sometimes referred to as OEC). OEG cells normally surround and protect neurons that are part of the olfactory system and assist those neurons in first developing and then repairing themselves if needed. They can secrete “growth factors” that stimulate neuronal growth. OEG cells also provide a track or framework on which the neuron grows. The fact that olfactory neurons, unlike neurons in the central nervous system, can repair themselves is one reason researchers are studying them.
A team headed by Dr. Carlos Lima in Lisbon, Portugal, has surgically transplanted olfactory cells (which the team refers to as olfactory mucosal tissue) into over 70 individuals (as of December 2005) with spinal cord injuries which had occurred anywhere from six months to six years prior to the surgery. A surgeon first extracts the cells from the nasal sinus (which may affect the person’s sense of smell). Because the olfactory cells are obtained from the patient into whom they will be transplanted, there is no problem with transplant rejection. Another advantage is that the progenitor stem cells only differentiate into cells that are part of the nervous system, including neurons and OEG cells. Consequently, it is hoped that these stem cells will form new neurons when they are transplanted.
In transplanting the olfactory cells, surgeons first remove scar tissue
in the area of the spinal cord injury. The olfactory cells are then placed
in the cavity created. Dr. Lima estimates that approximately 400,000 progenitor
stem cells are transplanted, together with 4 million neurons and millions
of OEG cells and immature neurons. The surgery is experimental and the
Lisbon team has not yet published articles describing its findings. However,
the physicians have indicated that while there have been no dramatic cures,
there has been improvement with many, but not all, patients. Improvement
ranges from increased sensation or decreased pain to improved motor abilities
or bowel and bladder function. Dr. Lima’s team is collaborating
with the Detroit Medical Center in treating American spinal cord injury
survivors. Because the FDA has not yet approved the procedure, Dr. Lima’s
team operates on patients in Portugal and the Detroit Medical Center performs
follow-up rehabilitation. The cost of surgery is around $50,000 (not including
travel costs). The cost of rehabilitation is between $3,000 and $4,000.
(1) A South Korean’s claims to have cloned human embryos have been at least partially discredited. One company has managed to transplant human DNA into a cell that divided several times but then stopped growing.
More on Stem Cell Research into SCI Therapy