Evaluation and Initial Treatment of Spinal Cord Injury
The primary assessment of a patient with trauma in the field follows
the ABCD prioritization scheme:
- Airway
- Breathing
- Circulation
- Disability (neurologic status). If the patient has a head injury,
is unconscious or confused, or complains of spinal pain, weakness, and/or
loss of sensation, then a traumatic spinal injury should be assumed.
Extreme care should be taken to allow as little movement of the spine
as possible to prevent more cord injury.
Any patient that has sustained a head injury and appears confused or is unconscious should be considered to have a traumatic spinal injury. If the patient is alert and indicates they have spinal pain, numbness or weakness the first responders also make the cautious assumption of an SCI. Any presumed spinal injury should be handled with extreme care and the patient should be immobilized.
Using a log-roll technique, the paramedics or other responders place the patient onto a backboard for transfer and ft the patient with a rigid cervical collar.
Hospital emergency departments follow the same ABCD scheme when evaluating SCI patients. Injuries that are life-threatening - e.g. breathing difficulties, systematic bleeding, a pneumothorax - take priority over the presumed spinal injury.
- Standard vital signs that include blood pressure, temperature, heart rate and respiratory status should be monitored. Using capnography as a respiratory status monitor is standard emergency department procedure.
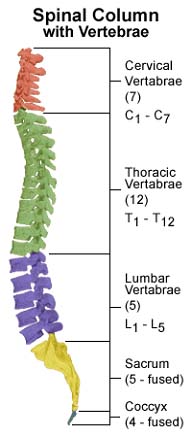
- A patient that has endured an injury high on the cervical cord may have difficulty breathing. These patients may need airway suction or intubation in order to get adequate air. Approximately one-third of those who have suffered a cervical injury need mechanical respiratory support. Using rapid-sequence intubation with in-line spinal immobilization is the ideal method when an airway is needed immediately. In cases where time is not a factor, a fiber optic laryngoscope intubation method is generally a safer option.
- Hypotension is possible because of a loss of blood caused by other injuries. Blood pooling in the extremities that are lacking sympathetic tone due to the interruption of the autonomic nerve system can also cause hypotension. The resulting hypoperfusion can cause permanent damage. Medical personnel sometimes elevate the legs and head. A blood transfusion or vasoactive medications may be necessary.
- The medical team does not remove the immobilization of the neck and body until the spinal injury has been ruled on. The cervical collar, blocks, tape, straps and any athletic headgear remain in place until the ruling is in.
- The patient should be given a neurological exam as soon as possible. This determines the level and severity of an injury. The accidents that injure spines sometimes result in traumatic brain injuries, too, so patients’ mental status and cranial nerve function are assessed.
- The medical team evaluates bladder distention by palpation or ultrasound. The patient should have a urinary catheter inserted to avoid any further harm to the bladder caused by distentio