Many SCI survivors develop chronic pain after their injury – sometimes the onset does not occur until years later. It’s estimated that about 30% of patients have chronic pain that affects the quality of life. This pain is both out-of-the-blue and in response to something. Pain that arises from the nervous system subjectively comes across as stabbing or burning and the patient often finds it difficult to pinpoint where the pain is coming from. Musculoskeletal pain by contrast is duller and easier for the patient to specify the place from. This type of pain is better understood and treatable, whereas neurogenic pain seems to observers to make the patient hyperexcitable and is poorly understood.
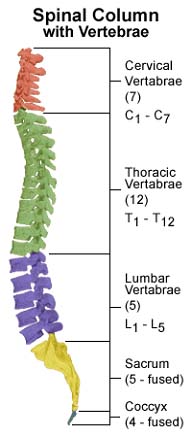
Neurologists distinguish between two types of neurogenic pain syndromes, referring to the point of injury in the spine. At-level pain is in segments at the level of SCI and below-level pain occurs at lower points on the spine and in nerves emanating from that area. At-level pain involves injury to nerve roots and dorsal gray brain matter. Below-level pain is tied to spinothalamic tracts.
How do doctors address pain in SCI patients? The same type of pain relief medications used for other conditions – analgesic drugs including opiates – are used. Antiepileptic drugs are prescribed because they might reduce pain by suppressing neuronal hyperexcitability in SCI patients. Antidepressant medications have been attempted, but for the most part they don’t work.
More out-there pain relief techniques have been attempted Much work has been done in intervening in the body with deep bra in stimulation and motor cortex stimulation. There are also techniques where surgeons attempt to disable parts of the spinal cord that are thought to conduct pain from problem areas. DREZ lesion therapy is also attempted. This stands for dorsal root entry zone lesions and is another technique neurosurgeons use to stop pain.