Trauma patients suspected of suffering an SCI usually get analyzed through high-tech imaging. Cervical collars are not removed until the images are read. If a patient does not exhibit neurological deficits, is alert and not confused, does not complain of any midline pain or tenderness, and is not intoxicated, the medical personnel may choose to remove the collar before the image assessment is made.
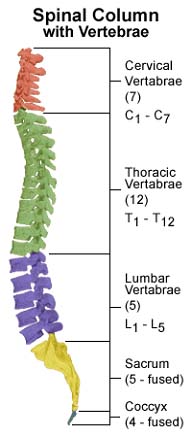
Plain x-rays for a quick assessment of fractures, alignment and soft tissue swelling is typically the first method used to evaluate a spinal cord injury. Because CT and MRI machines are widely available now, old fashioned radiography plays a lesser role in SCI diagnosis than it once did. Anteroposterior, open-mouth odontoid and lateral views are included in a complete x-ray set. If a lateral mass or facet injury is suspected, an oblique view may be required. An evaluation must include a visual check of all cervical vertebrae and the top of T1. If the lower vertebrae and T1 are not seen, a swimmer’s view should be used.
Neurological signs and/or symptoms seen in a set of normal x-rays often trigger further imaging with more advanced techniques.
CT scanning have a higher sensitivity for detecting spinal fractures. A CT can be done without moving the patient from the supine position. This method can also look for potential head injuries at the same time.
Abnormalities viewed in the first CT are reevaluated with a more detailed scan. If a spinal cord injury is suspected, patients who appear to have normal plain x-rays should undergo CT scanning for verification. The CT can also assess the patency of the spinal cord.
Both MRI and CT angiography can help doctors see the blood vessels around the spine. MRI is particularly useful for producing a look at the insides of the spinal cord.
Magnetic resonance imaging - An MRI is ideal for viewing intervertebral discs, spinal ligaments, paraspinal soft tissues and can better detect epidural hematomas than a CT scan. The CT is better used for assessing bone structures. An MRI is not sensitive to cord damage during the early stages of a spinal injury. An MRI may also interfere with pacemakers and metal inside the body. Because a patient is enclosed within an MRI, monitoring vital signs is difficult and ensuring the patient can breath is difficult.
Spinal cord injury without radiographic abnormality (SCIWORA) is a classification for patients with a suspected spinal cord injury without evidence of a vertebral injury on plain x-rays or CT. One explanation for this type of occurrence is a transient ligamentous deformation with spontaneous reduction. Children are more prone to this due to weak paraspinal muscles. People with lax soft tissue and elastic spinal ligaments are more prone to SCIWORA. Other conditions that may be responsible include epidural or intramedullary hemorrhage, radiographically occult intervertebral disc herniation, fibrocartilaginous emboli as a result of an intravertebral ruptured disc into the radicular artery or traumatic aortic dissection with spinal cord infarction.
Myelography is an imaging technique which involves the intrathecal instillation of contrast medium and shows its passage in the lumbar or cervical subarachnoid space around the spinal cord and nerve roots. Myelography uses a real-time form of X-ray called fluoroscopy. The contrast medium is a specially formulated water-soluble iodine-containing material.
CT myelography: CT scan is performed after myelography. Combining CT scan with myelography gives a better view of spinal cord and roots which appear as filling defect in the opaque subarachnoid space.
Low-dose CT myelography: The CT scan is performed with a relatively small amount of dilute contrast medium and thus has advantage of reducing radiation exposure as well as exposure to contrast media. This technique has largely replaced the conventional myelogram. Newer CT scan with multidetector scanners are being used now a days, which quickly reform the images equivalent to traditional myelography projections.
Myelography can be used to detect abnormalities of spinal cord, spinal canal and spinal nerve roots. Myelography can also diagnose the spinal stenosis and herniation of intervertebral disc into spinal canal.
Myelography has largely been replaced by CT myelogram and MRI scans for the diagnosis of spinal cord diseases. There are a few conditions for which conventional myelography is still used, such as suspected meningeal or arachnoid cyst.
A myelogram is also helpful in assessing the outcome of surgery in an individual patient and thus helps in planning surgery. Conventional myelography and CT myelography provide highly precise information before the surgeries like spinal fusion and spinal fixation.
Contraindications: Myelography is a quite safe technique but care should be taken in following conditions:
Complications: the most frequent complications are
Other resources:
Hopkins Medicine on myelograms
Use of myelograms in spinal cord birth injuries