 Years ago doctors made diagnoses from the visible signs of osteoporosis (lost height, dowager's hump, thin frame) and especially from bone fractures. Older people, especially women, who broke bones were often assigned a diagnosis of osteoporosis.
Years ago doctors made diagnoses from the visible signs of osteoporosis (lost height, dowager's hump, thin frame) and especially from bone fractures. Older people, especially women, who broke bones were often assigned a diagnosis of osteoporosis.
That has changed with the advent of modern imaging techniques. In particular, the Dual Energy X-ray Absorptiometry (DEXA) test has become the most important element of osteoporosis diagnosis. DEXA tests measure the density of bones. There is a lot more to the bone strength than density of course, but DEXA is so noninvasive and 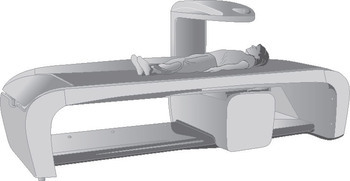 so fast that it has become pervasive. Bone density decline isn’t just a diagnostic factor; bone density has become the endpoint for treatment assessment in both trials for new treatments and in clinical practice.
so fast that it has become pervasive. Bone density decline isn’t just a diagnostic factor; bone density has become the endpoint for treatment assessment in both trials for new treatments and in clinical practice.
Indeed, the very definition of osteoporosis has now changed so that bone density is the main factor. Although the word osteoporosis was first used in 19th Century France and imported to English in the early 20th Century, a consensus criteria for diagnosis of osteoporosis did not exist until 1993.
The diagnostic process produces a measure of the bone density and compares it to a standard. If the density is too low, the person is most likely given a diagnosis of osteoporosis. Of course, a doctor must still assign such a diagnosis from all available evidence, but at this point the DEXA result is the dominant factor in most diagnoses.
DXA measures density of bones in hands very quickly fast. Other bones take a little more time. Patients must remove jewelry but not the process is as big a deal for preparation for an MRI. The correlation between bone density and bone strength is strong and mass is estimated to account for about 80% of strength. The other important factor is bone microarchitecture - the configuration of bony tissue at a microscopic level.
Broken bones are a red flag, for sure, and sometimes they will drive a diagnosis of osteoporosis even if the bone density is not in the danger range.
The reference bone density comes from a sample of bone densities of 30-year-old people. Separate data sets are collected for men and women. A distribution of densities is developed and a statistical profile. The distribution has a standard deviation (a standard deviation is a statistic about the data set). The measure of each person's bone density is compared to this distribution and the density is assigned a T-score. The T-score is the number of standard deviations from the mean. A bone density value 1.2 standard deviations above the mean is said to have a T-score of 1.2. A value 0.4 standard deviations below the mean has a T-score of -0.4.
If we call bone density BMD and the normal density in young adults YN with a standard deviation SD, then
T = (BMD – YN)/SD
Bone density tests sometimes report Z-scores. This is the number of standard deviations from the mean compared to a reference set taken from people of the same age. The T-score, by contrast, compares the bone density of a person, regardless of age, to the distribution of densities from 30-year-olds.
The current major sign of osteoporosis is a T-score below -2.5. So a T-score of -2.3 is not osteoporosis, but a T-score of -2.7 is osteoporosis.
Of course, few 30 year-olds have a bone density more than 2.5 standard deviations below the mean. But plenty of 70 year-olds have a bone density more than 2.5 standard deviations below the mean calculated from a data set from 30 year olds.
Osteopenia is a name assigned to condition when the bone density is low but not low enough to be osteoporosis. Osteopenia is generally said to be when the T-score is between -1 and -2.5.
Another problem with the focus on BMD is that many fractures happen in people without a T-score that would qualify as osteoporosis. An article published in the Journal of Bone and Mineral Research in 2014 said that half of fractures occur in “individuals with nonosteoporotic BMD”. (These are fragility fractures.)
| T-Score | What it means |
| -1 or higher | Normal |
| Between -1 and -2.5 | Osteopenia |
| -2.5 and lower | Osteoporosis |
Because we have better methods today. Old fashioned X-ray imaging is okay for some medical procedure and analyses, but it does not have the sensitivity to be useful in determining bone thinning. Radiologists have found bones must lose over 30% of mass before the demineralization is evident on a plain film x-ray.
 Diagnosis of osteoporosis will likely include a physical examination complete with x-rays. The physician may notice a loss of height, which is compounded by a "dowager's hump". This hump or curve of the spine is an indicator that bones are less dense than they need to be to fight off the manifestation of osteoporosis, and a bone density test will be the ultimate confirmation.
Diagnosis of osteoporosis will likely include a physical examination complete with x-rays. The physician may notice a loss of height, which is compounded by a "dowager's hump". This hump or curve of the spine is an indicator that bones are less dense than they need to be to fight off the manifestation of osteoporosis, and a bone density test will be the ultimate confirmation.
Unfortunately, biomarkers of bone turnover are not well understood or provide too weak a symbol to be of practical use as a warning sign for osteoporosis.
Depending on your overall physical health and any symptoms, the doctor may wish to test vitamin D and/or calcium levels in the blood. There are other biomarkers associated with bone turnover, and in the future they may be used widely in the diagnosis of osteoporosis.
Gait speed is often used as a measure of how well a person is holding up to old age. Doctors may consider it when formulating a diagnosis of osteoporosis.
Most patients have a low body mass index well before they have a Dowager’s Hump. Hence, it is really DEXA or another scan that identifies osteoporosis. Patient history and physical examination, however, are useful for figuring out if the osteoporosis has an identifiable cause - i.e. is secondary osteoporosis.
The medical profession has criticized itself for looking too much at BMD and ignoring other risk factors for fracture. Some encourage doctors to consider other data and to remember that osteoporosis is a systemic skeletal disease, not just a local problem with individual bones. Although the hallmark fractures of osteoporosis are in the vertebrae, forearm and upper leg, low trauma fractures anywhere in the skeleton can be associated to low bone density.
Given that is so difficult to assess and quantify bone microarchitecture in the living body and that doctors want to prevent fractures before they happen and that DXA scans are inexpensive, the BMD will probably continue to be the first diagnosis tool.
Osteoporosis is a silent disease so some sort of scientific diagnosis is needed to detect and stop the onset and progression of the disease.
The British company ClinRisk publishes a website that estimates the risk of fracture due to osteoporosis. Their proprietary copyrighted algorithm – which is not explained on their site – uses patient information about age, medicine and alcohol usage, BMI, and more. It reports an estimate of a bone fracture in the next 10 years.
This may be useful and interesting for some people, but it should not substitute for a visit to the doctor’s office.
